NB More complex knowledge about Inflammaging at http://biopsychosocialmedicine.com/projects/senior-health/senoinflammation-or-inflammaging-or/
Ongoing work – not at all ready to read! please see http://carism.se/notes/inflammaging-in-general-and-ear-nose-throat-in-particular/ until the below is ready to be read!
Upcoming Swedish headline = Inflamaging in general and examples in Ear-Nose-Throat areas
NOTE Warning – below is a first draft (which is updated when I can work without the hindrance of severe tinnitus syndrome) so read with caution (even because of my dyslexia).
The intention is only that the below can give some text to afterthoughts but also afterwards tips how to influence both rhinosinuit and tinnitus, given there is precisely a connection where the rhinosinuiut is the source of complicated tinnitus via dysfunctional ear trumpet ……
One more warning; some information below is probably too many surprising and perhaps even more worrying! See * a few lines below
NB! If you who read above feel insecure, please email me at info@stressmedicin.se – above is not easy to understand, given you do not have in-depth science-knowledge- and clinically based education!
* But sometimes new knowledge challenges what we may have taken for granted, which may turn out to be destructive. It is then important to critically review also when it comes to completely new perspectives, see e.g. Paradigm | Biopsychosocial Medicine or the problems around Confirmation bias (basically = what you already believe – within your private/scientific/clinical paradigm, do you think is right), A huge problem for health care? Confirmation bias, placebo/nocebo vs reductionistic medicine | Biopsychosocial Medicine – A major problem in principle in all education is that many perceive the knowledge (and related practice) that is taught is precise knowledge, which it is not without varying degrees of “safe knowledge”. Even worse is if the teacher believes that this (e) teaches absolute knowledge without varying degrees of deficientness which the teacher himself more or less understood. Note it is not black and white, if you cross a street with traffic all the time, you should not go straight out without looking for! The same applies to all types of learning – it is important to look for and critically review before accepting the “paradigm” that is taught – see above link! NB! If you who read above feel unsure, please email me at info@stressmedicin.se – above is not easy to understand, given you do not have in-depth venskaps-based training!
Inflamm-aging. An evolutionary perspective on immunosenescence
(2000) “In this paper we extend the ”network theory of aging,” and we argue that a global reduction in the capacity to cope with a variety of stressors and a concomitant progressive increase in proinflammatory status are major characteristics of the aging process. This phenomenon, which we will refer to as ”inflamm-aging,” is provoked by a continuous antigenic load and stress. On the basis of evolutionary studies, we also argue that the immune and the stress responses are equivalent and that antigens are nothing other than particular types of stressors. We also propose to return macrophage to its rightful place as central actor not only in the inflammatory response and immunity, but also in the stress response”. https://pubmed.ncbi.nlm.nih.gov/10911963/
(2020) – Age-related cerebral small vessel disease and Inflammaging – https://www.nature.com/articles/s41419-020-03137-x?elqTrackId=c172648eefc748deae1322fee525e44c see PDF
“The continued increase in global life expectancy predicts a rising prevalence of age-related cerebral small vessel diseases (CSVD), which requires a better understanding of the underlying molecular mechanisms. In recent years, the concept of “inflammaging” has attracted increasing attention. It refers to the chronic sterile low-grade inflammation in elderly organisms and is involved in the development of a variety of age-related chronic diseases. Inflammaging is a long-term result of chronic physiological stimulation of the immune system, and various cellular and molecular mechanisms (e.g., cellular senescence, immunosenescence, mitochondrial dysfunction, defective autophagy, metaflammation, gut microbiota dysbiosis) are involved. With the deepening understanding of the etiological basis of age-related CSVD, inflammaging is considered to play an important role in its occurrence and development. One of the most critical pathophysiological mechanisms of CSVD is endothelium dysfunction and subsequent blood-brain barrier (BBB) leakage, which gives a clue in the identification of the disease by detecting circulating biological markers of BBB disruption. The regional analysis showed blood markers of vascular inflammation are often associated with deep perforating arteriopathy (DPA), while blood markers of systemic inflammation appear to be associated with cerebral amyloid angiopathy (CAA). Here, we discuss recent findings in the pathophysiology of inflammaging and their effects on the development of age-related CSVD. Furthermore, we speculate the inflammaging as a potential target for future therapeutic interventions to delay or prevent the progression of the age-related CSVD.”
NB above can be understood somwhat different depending on what paradigm is used as platform. I clarify how we define the paradigm of Biopsychosocial Stress Medicine at Definition | Biopsychosocial Medicine
Inflamm-aging: the missing link to COVID-19 age-related mortality?
The possible pathophysiology mechanism of cytokine storm in elderly adults with COVID-19 infection: the contribution of “inflame-aging”
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7289226/
“The aim of the present review was to summarize experimental data and clinical observations that linked the pathophysiology mechanisms of “inflamm-aging”, mild-grade inflammation, and cytokine storm in some elderly adults with severe COVID-19 infection.”
Covid-19 hyperinflammation and post-Covid-19 illness may be rooted in mast cell activation syndrome
https://www.sciencedirect.com/science/article/pii/S1201971220307323
Innehåll
Motivering till texterna nedan
Kort tinnitus syndrom översikt
Inflammaging generellt
Inflammaging och hörseldysfunktioner
Mast cell activation syndrome, Inflammaging and tinnitus
Kronisk Rinosinuitis tKRS) och inflammaging
Ethmoid sinus – chronic and acute
Mast cell activation synrome
NO and …
Vargata
Sinuit, speciellt maxillaris typ 2 utan symptom
Mer om sinuit syndrom
Tyst Sinuit
Sinuitis och örontrumpeten
Mer om örontrumpeten och dess funktioner
Mellan örats problematik
”Ear fullness”
More complex knowledge about inflammaging
Länkar
Motivering till texterna nedan.
Flera skäl;
1. Just inflammaging har speciella konsekvenser för de flesta dysfunktioner som vi först sista tiden börjar (!) förstå – och sannolikt en del tinnitus varianter, speciellt de som relaterar till rinosinuit som ”källa”.
2. Nedan skriver jag av minst 4 skäl bl.a. eftersom mitt områden inte är vad jag skriver nedan utan psykofysiologisk stressmedicin så befinner jag mig på något ”djup vatten” – liksom också att jag fokuserar på min egen komplexa, svåra tinnitus syndrom variant där jag fått arbete mycket i ”blindo” i stort sett utan professionella diagnoshypoteser och biologiska åtgärdsprogram:
(a) inom vårt område så har vi välutvecklade instrument och verktyg för diagnoshypotesbildning baserat på vanligen omfattande utredningar liksom också biopsykosocial medicinsk verktygslåda som varje patient via grupputbildning jobbar med för att i samverkan med handledande kliniker skräddarsy sin användning av verktygen (manual ”Patient som rimligen kompetent aktiv resurs och medarbetare i sin egen rehab”)
(b) vilket uppenbarligen inte är fallet inom de olika komplexa tinnitus syndromområdena där baskunskaperna uppenbarligen är ytterst begränsade i vårt land (har gärna fel här!). medan internationellt är under markant utveckling utifrån olika multidisciplinära perspektiv – detta motiverar mig att åtminstone försöka skapa mig ett system integrerad multidisciplinär praktiskt användbart perspektiv/bild av Tinnitus syndromen.
(c) eftersom jag själv utifrån patientperspektivet kämpar fortfarande med mycket svårt (som alltså jag anser (tyvärr!) inte välkänt och med ytterst bristfällig kunskaps- och praktikplattform, speciellt i Sverige) Tinnitus Syndrom men tror nu att min hälsa kan återställas – med egeninsatser – priviligierad som jag är utifrån mina kliniska erfarenheter att arbeta med komplicerade kliniska multifaceterade dysfunktioner!
(d) ovan gör att jag kämpar på flera fronter tämligen även jag ”bild” i avsaknad av remiliga utredningsinstrument och åtgärdsprogram – vilket manar till stor försiktighet i vad jag skriver nedan! Dessutom är de internationella ansatser jag bygger på ofta fragmentariska och få ansatser har gjorts att försöka göra en systemintegrerande multidisciplinär kunskaps- och praktikplattform att utgå ifrån.
Samtidigt är behovet (avseende svår tinnitus) uppenbarligen mer omfattande än vad som samhällsmedicinska företrädare förstått – där dock detta problemområde inte är ensamt att vara i stort sett bortglömt eller marginaliserat – uppenbarligen! Se t.ex. https://carism.se/projekt-carism/urgent-needed-knowledge-and-practice-development-different-kinds-of-tinnitus/ – OBS som också den sidan är under utveckling – samtidigt som jag är ytterst handikappad att kunna arbete mer än korta stunder pga handikappande Tinnitus Syndrom problem.
Kort tinnitus syndrom översikt
Tinnitus syndrom kan var orsakat av en eller flera olika ”källor”, ofta flera även om en kan vara vid orsak vid uppstart! Det kan relatera till många olika system/processer och biologiska dysfunktionella lokalisationer och relationer, inte sällan multifaceterade/multidisciplinära och ej väl kunskaps- och praktiskbaserade. Även om vi inte utgår ifrån absolut kunskap inom egentligen något område så är tinnitusområdena (pluralis!) ovanligt bristfälliga. Detta diskuterar jag på andra sidor, t.ex. http://carism.se/projekt-carism/urgent-needed-knowledge-and-practice-development-different-kinds-of-tinnitus/
Eftersom jag själv haft hanterbar bullerskade tinnitus i 60 år men sedan oktober 2019 plötsligt (diskuterar hur det sannolikt uppstod – på andra sidor) mycket svårt med ”flera inre larm kluster” – och mycket svårt att leva med, så har jag av överlevnadsskäl fokuserat på att försöka pussla ihop (inte allt men) mycket, ofta fragmentariskt internationellt som sker – för att få en angripbar multidisciplinär hypotesdiagnos att arbeta efter. Eftersom min styrka är kreativitet, innovation och inte ”ge mig”, så resulterar detta i en allt mer vidareutvecklad verktygslåda som faktiskt bygger vidare på min egen doktorsavhandling 1986.
Nedan berör en av de viktigast källorna till min svåra Tinnitus – som jag skulle ha kunnat ha insett redan för ett år sedan, d.v.s. om jag själv haft nedan kunskap inte bara om tyst Kronisk RinoSinuit (tKRS) utan också dess potentiella källa till svår tinnitus.
Fokus utifrån nuvarande kunskap utifrån begreppet ”Inflammaging” förklarar nog varför jag själv missat (tidigare) tKRS, trots jag även haft tillfälliga akuta reaktioner, tex. i samband med bastubad mycket kraftiga, märkliga symptom i hela huvudet för över ett år sedan!
OBS, igen att nedan är mycket rå, obearbetat (och oöversatt!) text och framför allt ej strukturerat på ett effektivt och hanterbart sätt! På annan plats skall jag sammanfatta min verktygslåda, men kan kort säga här att nedan ”tänk” lett till flera nya verktyg som verkar vara effektiva även för att påverka min fortfarande svåra tinnitus när jag fokuserar på KRS biobeteende ”rensning” – förutom allt övrigt, t.ex. också viktigt få ordning på KRSen!
https://www.researchgate.net/publication/326612330_Inflammaging_a_new_immune-metabolic_viewpoint_for_age-related_diseases
Nedan baseras bl.a. på viktiga utgångspunkter
(a) ”Inflammaging” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5675822/ &
(b) ”steroider ej lämpligt, ev. skadligt för äldre” (NB Unique form of chronic sinusitis in older patients – https://www.sciencedaily.com/releases/2019/01/190123105817.htm); ””We’re hoping this data will stimulate some interest in the elderly population with respect to chronic sinusitis management, because it suggests we may need patient-specific treatments targeting these older patients. That’s particularly important because steroids can have a number of short- and long-term adverse effects, and those side effects are much more likely in older patients than they are in younger patients,” said Turner.”
Alltså för mig ett nytt huvudproblemfokus (!) relaterat till svår tinnitus – som blir allt tydligare = ”tyst” kronisk rinosinuit, tKRS, som nu är ”ökat mindre tyst” sista månaden med t.ex. sub-kroppstemperatur förändringar under natten vid ökad slembildning (+ tinnitus-storm, som eg. ej ändrats sedan oktober 2019).
Nu till min ”oförbordade” (inte symfoni utan) samling av länkar;
-> Do Aging Factors Influence the Clinical Presentation and Management of Chronic Rhinosinusitis?
https://journals.sagepub.com/doi/abs/10.1177/0194599817691258?journalCode=otoj
“Age-dependent decrease in the levels of the S100 family proteins (https://pubmed.ncbi.nlm.nih.gov/32564786/) involved in epithelial proliferation, repair, and defenses combined with chronic inflammation might lead to an increased risk of abnormal microbial colonization and loss of microbiota diversity. Ultimately, these changes could have the potential to alter the physiopathology of CRS in the elderly.”
Inflammaging generallt
Se https://en.wikipedia.org/wiki/Inflammaging
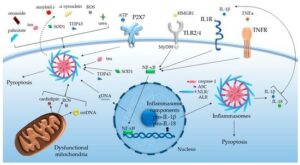
Inflamm-aging (also known as inflammaging or inflamm-ageing) is a chronic low-grade inflammation that develops with advanced age. It is believed to accelerate the process of biological aging and to worsen many age-related diseases.
Inflammaging is defined as low-grade chronic systemic inflammation established during physiological aging. Altered levels of proinflammatory cytokines (e.g., IL-6 and TNF-α), acute-phase reactants (C-reactive protein [CRP]), and decreases in IL-10 impair the maintenance of immunological homeostasis. Can Exercise Be an Immunotherapy? https://www.medscape.com/viewarticle/809935_7
An Update on Inflamm-Aging: Mechanisms, Prevention, and Treatment – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4963991/
“Liksom immunsvaret har inflammation en fysiologisk funktion i den normala kroppen. Måttliga inflammatoriska svar är fördelaktigt för kroppen men när överdriven, blir svaret skadligt. Förändringar i det inflammatoriska cytokinnätverket styr riktningen för inflammationsutvecklingen. Den dynamiska balansen i nätverket av proinflammatory cytokiner och antiinflammatoriska cytokiner upprätthåller den fysiologiska funktionen av inflammation i den normala kroppen. Tippa balansen från anti-inflammation till proinflammation kan leda till patologiska förändringar. Ihållande inflammation under inflamm-åldrandet kan orsaka inflammationsrelaterade sjukdomar.
Inflamm-åldrande är en avgörande faktor för åldrandets hastighet och av livslängd och är starkt relaterat till Alzheimers sjukdom [2], Parkinsons sjukdom, akut lateral skleros, multipel skleros, åderförkalkning, hjärtsjukdomar, åldersrelaterad makuladegeneration [14], diabetes typ II [15], osteoporos och insulinresistens [16], cancer, och andra sjukdomar. Inflamm-åldrande ökar också sjuklighet och dödlighet, avsevärt skadar hälsan hos patienter, och orsakar en nedgång i livskvaliteten för patienter [16]. Kronisk, subklinisk inflammation och immunsjukdomar samexisterar i processen för inflamm-åldrande. Epidemiologiska studier visar att med åldern finns det en obalans i förlusten av gammalt ben och bildandet av nytt ben. Inflamm-åldrande kan vara en av de bidragande faktorerna till obalansen och till den efterföljande överdriven förlust av ben. Inflammatoriska markörer av inflamm-åldrande ge kliniker med nödvändiga data för riskbedömning av osteoporos. Inflammatoriska cytokiner kan vara terapeutiska mål för att förbättra bildandet av ben hos äldre efter benoperationer [16]. Överdriven inflammation under inflamm-åldrande ökar sjuklighet och dödlighet hos patienter efter ben operationer, även om mekanismen för detta fortfarande oklart [17]. I processen för inflamm-åldrande, de patofysiologiska förändringar i tjocktarmen avslöjas på cell- och molekylära nivåer, och dessa kulminerar i inflammationen som leder till skada av magslemhinnan och epitel samt en minskning av epitels förmåga att regenerera [18] (figur 1).
Inflammaging: a new immune–metabolic viewpoint for age-related diseases – https://www.nature.com/articles/s41574-018-0059-4
Inflammageing: chronic inflammation in ageing, cardiovascular disease, and frailty https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6146930/
NB Unique form of chronic sinusitis in older patients https://www.sciencedaily.com/releases/2019/01/190123105817.htm
“With an initial goal of identifying subgroups of patients based on their inflammatory signature — the different cytokines and inflammatory proteins found in tissue or mucus — Vanderbilt investigators recognized that one of the identified subgroups was enriched in patients over age 60 “.
Inflamm‐aging: An Evolutionary Perspective on Immunosenescence 2006
https://nyaspubs.onlinelibrary.wiley.com/doi/epdf/10.1111/j.1749-6632.2000.tb06651.x
“Abstract: In this paper we extend the “network theory of aging,” and we argue that a global reduction in the capacity to cope with a variety of stressors and a concomitant progressive increase in proinflammatory status are major characteristics of the aging process. This phenomenon, which we will refer to as “inflamm‐aging,” is provoked by a continuous antigenic load and stress. On the basis of evolutionary studies, we also argue that the immune and the stress responses are equivalent and that antigens are nothing other than particular types of stressors. We also propose to return macrophage to its rightful place as central actor not only in the inflammatory response and immunity, but also in the stress response. The rate of reaching the threshold of proinflammatory status over which diseases/disabilities ensue and the individual capacity to cope with and adapt to stressors are assumed to be complex traits with a genetic component. Finally, we argue that the persistence of inflammatory stimuli over time represents the biologic background (first hit) favoring the susceptibility to age‐related diseases/disabilities. A second hit (absence of robust gene variants and/or presence of frail gene variants) is likely necessary to develop overt organ‐specific age‐related diseases having an inflammatory pathogenesis, such as atherosclerosis, Alzheimer’s disease, osteoporosis, and diabetes. Following this perspective, several paradoxes of healthy centenarians (increase of plasma levels of inflammatory cytokines, acute phase proteins, and coagulation factors) are illustrated and explained. In conclusion, the beneficial effects of inflammation devoted to the neutralization of dangerous/harmful agents early in life and in adulthood become detrimental late in life in a period largely not foreseen by evolution, according to the antagonistic pleiotropy theory of aging.”
Health relevance of the modification of low grade inflammation in ageing (inflammageing) and the role of nutrition https://www.sciencedirect.com/science/article/pii/S156816371730003X
…”We conclude that slowing, controlling or reversing Low Grade Inflammation (LGI) is likely to be an important way to prevent, or reduce the severity of, age-related functional decline and the onset of conditions affecting health and well-being; that there is evidence to support specific dietary interventions as a strategy to control LGI; and that a continued research focus on this field is warranted.”
Inflammaging and Anti-Inflammaging: The Role of Cytokines in Extreme Longevity https://link.springer.com/article/10.1007/s00005-015-0377-3 –
Immune Senescence and Inflammaging Mini-Review https://www.bio-rad-antibodies.com/immune-aging-senescence.html
Mast Cells, Neuroinflammation and Pain in Fibromyalgia Syndrome https://www.frontiersin.org/articles/10.3389/fncel.2019.00353/full
“Fibromyalgia Syndrome (FMS) is a disorder of chronic, generalized muscular pain, accompanied by sleep disturbances, fatigue and cognitive dysfunction. There is no definitive pathogenesis except for altered central pain pathways. We previously reported increased serum levels of the neuropeptides substance P (SP) and its structural analogue hemokinin-1 (HK-1) together with the pro-inflammatory cytokines IL-6 and TNF in FMS patients as compared to sedentary controls. We hypothesize that thalamic mast cells contribute to inflammation and pain, by releasing neuro-sensitizing molecules that include histamine, IL-1β, IL-6 and TNF, as well as calcitonin-gene related peptide (CGRP), HK-1 and SP. These molecules could either stimulate thalamic nociceptive neurons directly, or via stimulation of microglia in the diencephalon. As a result, inhibiting mast cell stimulation could be used as a novel approach for reducing pain and the symptoms of FMS”. https://www.mdpi.com/2073-4409/9/7/1565/htm Mitochondrial Dysfunction and Inflammaging in Heart Failure: Novel Roles of CYP-Derived Epoxylipids
https://www.mdpi.com/2073-4409/9/7/1565/htm Mitochondrial Dysfunction and Inflammaging in Heart Failure: Novel Roles of CYP-Derived Epoxylipids
Mast Cells (Part 3): The Mast Cell-Glia Interaction In Chronic Inflammation

The more inflammation happens, the more that mast cells and glia communicate and create stronger bonds/crosstalk.
https://mybiohack.com/blog/mast-cells-glia-sali-cirs
Immunosenescence, Inflammaging, and Their Implications for Cancer and Anemia https://link.springer.com/chapter/10.1007/978-981-13-3585-3_14
Special Issue ”Inflammaging and Oxidative Stress in Aging and Age-Related Disorders”
https://www.mdpi.com/journal/ijms/special_issues/inflammaging_oxidative_stress
The interplay between immunosenescence and age-related diseases https://link.springer.com/article/10.1007/s00281-020-00806-z
Aging is a major risk factor for the higher incidence and prevalence of chronic conditions, such as cardiovascular diseases, metabolic diseases, and neurodegenerative diseases. Chronic systemic sterile inflammation is crucially involved with the etiology and progression of these conditions [1]. Several features of premature aging have been reported in young adults or adults with these chronic conditions (Fig. 1). In the elderly, these conditions are often presented with multimorbidity and may finally lead to organ failure and death. With the advance of immunosenescence (aging of the immune system), older adults also become more susceptible to infectious diseases and cancer. Elderly population is at increased risk for developing and dying from influenza and coronavirus disease 2019 (COVID-19). Of note, the adults with chronic (inflammatory) conditions are the ones with heightened risk for developing severe COVID-19 and dying [2]. Therefore, there is an interplay between immunosenescence and age-related diseases. In this way, it is important to intervene more quickly and multidimensionally with novel preventive and therapeutic approaches. The study of immunosenescence can bring viable solutions for the prevention and treatment of these diseases as well as to increase the healthspan of elderly populations.
Multiple mechanisms of accelerated aging are similarly found in age-related diseases. Abbreviations: CMV, cytomegalovirus; SASP, senescence-associated secretory phenotype
Inflammaging och hörseldysfunktioner
Google att söka “Inflammaging cronic sinus tinnitus” + “can chronic sinus cause tinnitus”
Resolution of Inflammation (including Inflammageing) and Age-Related Hearing Loss (ARHL)
https://www.frontiersin.org/articles/10.3389/fncel.2017.00192/full – https://escholarship.org/content/qt45h1k38c/qt45h1k38c_noSplash_5fcccc3f6510d1bfd6388b48ff30fee7.pdf
“Another key contributor to several age-related diseases, including ARHL, is the state of chronic inflammation in the elderly known as ‘‘inflammaging’’ (Capri et al., 2006; Hunt et al.,
2010; Leng et al., 2011; Baylis et al., 2013; Verschuur et al., 2014). Inflammaging is a consequence of immune-senescence, the aging of the immune system (Capri et al., 2006; Hunt et al., 2010).
A potential link with inflammaging may be very important for ARHL, providing new approaches to prevent the development of this condition.
As a matter of fact, ARHL severity has already been linked to some factors associated with inflammation and inflammaging (Gates et al., 1993; Gates and Mills, 2005; Frisina et al., 2006;
Verschuur et al., 2014). For instance, it has been shown that spiral ganglion cell damage can be caused by changes in the immune system (Iwai et al., 2003, 2008), while vascular and metabolic changes may affect the stria vascularis and, indirectly, cause inflammatory damage (Saitoh et al., 1995; Ohlemiller, 2009; Fetoni et al., 2011). In a clinical trial an association was
found between serum immunoglobulin G and hearing loss in individuals over 60 years of age (Lasisi et al., 2011). Thus, there is a high probability that inflammation and inflammaging could
play a role in ARHL.”
Tinnitus, hearing loss and inflammatory processes in an older Portuguese population – https://www.tandfonline.com/doi/abs/10.1080/14992027.2019.1698775?needAccess=true&journalCode=iija20
“Conclusions: The results of our study showing fluctuations in inflammatory markers along the hearing loss process, reinforce the idea that inflammatory mechanisms are involved in hearing loss pathogenesis but also in tinnitus. IL10 levels appear significantly altered in tinnitus but not in hearing loss.”
https://www.tandfonline.com/doi/abs/10.1080/14992027.2019.1698775?scroll=top&needAccess=true&journalCode=iija20 “Conclusions: The results of our study showing fluctuations in inflammatory markers along the hearing loss process, reinforce the idea that inflammatory mechanisms are involved in hearing loss pathogenesis but also in tinnitus. IL10 levels appear significantly altered in tinnitus but not in hearing loss.”
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5675822/ Chronic Inflammation – Imflammaging – in the Ageing Cochlea: A Novel Target for Future Presbycusis Therapy – “Chronic, low-grade inflammation, or Inflammaging, is a crucial contributor to various age-related pathologies and natural processes in aging tissue, including the nervous system. Over the past two decades, much effort has been done to understand the mechanisms of Inflammaging in disease models such as type II diabetes, cardiovascular disease, Alzheimer’s disease, Parkinson’s disease, and others”. BvS And TINNITUS – same link also https://www.researchgate.net/publication/320354252_Chronic_Inflammation_-_Inflammaging_-_in_the_Ageing_Cochlea_A_Novel_Target_for_Future_Presbycusis_Therapy
See also – https://journals.plos.org/plosbiology/article?id=10.1371/journal.pbio.3000307 Neuroinflammation mediates noise-induced synaptic imbalance and tinnitus in rodent models
Also https://www.mdpi.com/journal/ijms/special_issues/Molecular_Hearing_Loss
Chronic Inflammation – Inflammaging – in the Ageing Cochlea: A Novel Target for Future Presbycusis Therapy https://www.researchgate.net/publication/320354252_Chronic_Inflammation_-_Inflammaging_-_in_the_Ageing_Cochlea_A_Novel_Target_for_Future_Presbycusis_Therapy
“Chronic, low-grade inflammation, or inflammaging, is a crucial contributor to various age-related pathologies and natural processes in aging tissue, including the nervous system. Over the past two decades, much effort has been done to understand the mechanisms of inflammaging in disease models such as type II diabetes, cardiovascular disease, Alzheimer’s disease, Parkinson’s disease, and others. However, despite being the most prevalent neurodegenerative disorder, the number one communication disorder, and one of the top three chronic medical conditions of our aged population; little research has been conducted on the potential role of inflammation in age-related hearing loss (ARHL). Recently, it has been suggested that there is an inflammatory presence in the cochlea, perhaps involving diffusion processes of the blood-brain barrier as it relates to the inner ear. Recent research has found correlations between hearing loss and markers such as C-reactive protein, IL-6, and TNF-α indicating inflammatory status in human case-cohort studies. However, there have been very few reports of in vivo research investigating the role of chronic inflammation’s in hearing loss in the aging cochlea. Future research directed at better understanding the mechanisms of inflammation in the cochlea as well as the natural changes acquired with aging may provide a better understanding of how this process can accelerate presbycusis. Animal model experimentation and pre-clinical studies designed to recognize and characterize cochlear inflammatory mechanisms may suggest novel treatment strategies for preventing or treating ARHL. In this review, we seek to summarize key research in chronic inflammation, discuss its implications for possible roles in ARHL, and finally suggest directions for future investigations.”
(ev. tyst) Kronisk Rinosinuitis tKRS) och inflammaging
Do Aging Factors Influence the Clinical Presentation and Management of Chronic Rhinosinusitis?
https://journals.sagepub.com/doi/abs/10.1177/0194599817691258?journalCode=otoj
“Age-dependent decrease in the levels of the S100 family proteins (https://pubmed.ncbi.nlm.nih.gov/32564786/ – https://www.researchgate.net/requests/r81831782) involved in epithelial proliferation, repair, and defenses combined with chronic inflammation might lead to an increased risk of abnormal microbial colonization and loss of microbiota diversity. Ultimately, these changes could have the potential to alter the physiopathology of CRS in the elderly.”
S100 family proteins in inflammation and beyond https://www.researchgate.net/publication/340723108_S100_family_proteins_in_inflammation_and_beyond printout requeted
Ethmoid sinus – chronic and acute
1939 –
OBSCURE LOW GRADE CHRONIC INFECTIONS OF THE ETHMOID SINUSES USE OF THE PROETZ DISPLACEMENT SUCTION FOR DIAGNOSIS
https://jamanetwork.com/journals/jama/article-abstract/286392
“The diagnosis of chronic infection of the ethmoid sinuses is one of the difficult diagnostic problems in rhinology. It is particularly difficult in those low grade chronic infections of the ethmoid sinuses in which the nasal passages appear normal on one or more examinations and in which any symptoms pointing directly to the sinuses are so slight as to be almost nonexistent and yet in which there is sufficient systemic absorption from the ethmoid infection to cause very definite systemic symptoms. It is these cases of obscure low grade infection to which I wish to call attention because they are so frequently overlooked.
Until a few years ago the diagnosis of chronic suppuration of the ethmoid sinuses depended on the examiner seeing pus coming from the middle or superior meatus after the maxillary, frontal or sphenoid sinus had been excluded as the source of the pus.”
SE –
Dold låg-gradig kronisk etmoid sinuit infektion – användning av ” Sinus Mapping by the Displacement Method” för diagnos (https://pubs.rsna.org/doi/10.1148/8.6.502)
https://jamanetwork.com/journals/jama/article-abstract/286392 Diagnos av kronisk infektion av ethmoid bihålorna är en av de svåraste diagnostiska problem i rhinology. Det är särskilt svårt i de låggradiga kroniska infektioner i ethmoid bihålorna där näsgångarna ses som normala på en eller flera undersökningar och där eventuella symtom som pekar direkt på bihålorna är så små att de är nästan obefintliga och ändå i vilka det finns tillräcklig systemisk absorption från ethmoid infektionen att orsaka mycket tydliga systemiska symtom. Det är dessa fall av ”tyst” (dold) låggradig infektion som jag vill uppmärksamma eftersom de är så ofta förbises.
Fram till några år sedan diagnos av kronisk suppuration av ethmoid bihålorna berodde på examinator ser var kommer från mitten eller övre meatus efter det maxillary, frontal eller sphenoid sinus hade uteslutits som källan till var” (även kolla (MRI) Evaluation of MRI range of fungal spherical rhinosinusitis http://gjzy.cintcm.com/en/oa/DArticle.aspx?type=view&id=202005008&utm_source=TrendMD&utm_medium=cpc&utm_campaign=International_Journal_of_Traditional_Chinese_Medicine_TrendMD_1
Bacteriology of Acute and Chronic Ethmoid Sinusitis https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1169095/
“Ethmoid sinusitis is a common infection. However, in contrast to maxillary sinusitis, the microbiology of ethmoid sinusitis is not well established; and only a few reports have documented the organisms isolated (1, 6, 9, 13). The role of anaerobes in this infection has also not been well studied, although the recovery of anaerobes was recorded in a few cases (13). This report describes the author’s experience in studying the aerobic and anaerobic microbiology of ethmoid sinusitis.”
Chronic ethmoidal sinusitis https://www.ncbi.nlm.nih.gov/medgen/3454 “Inflammation of the ethmoid sinus that typically lasts beyond eight weeks. It is caused by infections, allergies, and the presence of sinus polyps or a deviated septum. Signs and symptoms include headache, nasal discharge, swelling in the face, dizziness, and breathing difficulties”.
What to know about ethmoid sinusitis – https://www.medicalnewstoday.com/articles/327517
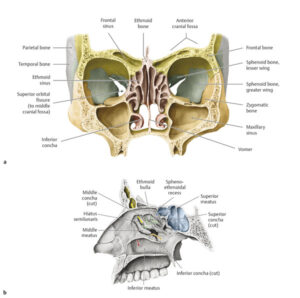
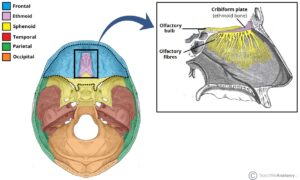
https://en.wikipedia.org/wiki/Ethmoid_sinus
The ethmoid sinuses or ethmoid air cells of the ethmoid bone are one of the four paired paranasal sinuses. The cells are variable in both size and number in the lateral mass of each of the ethmoid bones and cannot be palpated during an extraoral examination.[1] They are divided into anterior and posterior groups.[2] The ethmoid air cells are numerous thin-walled cavities situated in the ethmoidal labyrinth and completed by the frontal, maxilla, lacrimal, sphenoidal, and palatine bones. They lie between the upper parts of the nasal cavities and the orbits, and are separated from these cavities by thin bony lamellae
SE – Ethmoid bihålorna eller ethmoid luftceller av ethmoid ben är en av de fyra parade paranasala bihålorna. Cellerna är variabel i både storlek och antal i den laterala massan av var och en av ethmoid ben och kan inte palperas under en extraoral undersökning. [1] De är indelade i främre och bakre grupper. [2] Ethmoidluftcellerna är talrika tunnväggiga håligheter som ligger i den ethmformade labyrinten och kompletteras av frontal-, överkäke-, lacrimal-, sphenoidal- och palatinbenen. De ligger mellan de övre delarna av näshålorna och banorna, och separeras från dessa hålrum genom tunna beniga lameller
www.radiologykey.com/20-sinuses
https://teachmeanatomy.info/head/osteology/ethmoid-bone/ The ethmoid bone is a small unpaired bone, located in the midline of the anterior cranium – the superior aspect of the skull that encloses and protects the brain.
The microbiology of ethmoid and maxillary sinuses in patients with chronic sinusitis – https://pubmed.ncbi.nlm.nih.gov/12761703/ “.. Investigate aerob-anaerob microorganisms growth in maxillary and ethmoid sinuses by evaluating aspiration materials from patients with chronic sinusitis” (BvS) for diagnosis purpose
Bacteriology of Acute and Chronic Ethmoid Sinusitis https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1169095/ “Aspirates from 26 acutely and 17 chronically infected ethmoid sinuses were studied. Thirty-seven aerobes and 10 anaerobes were recovered from isolates from patients with acute sinusitis. Streptococcus pneumoniae and Haemophilus influenzae were predominant. Twenty-seven aerobes and 41 anaerobes were found in isolates from patients with chronic sinusitis. The predominant isolates were anaerobic gram-negative bacilli and Peptostreptococcus spp.”
Mer … Bakgrundsdokument rinosinuit – Läkemedelsverket –
Bakgrundsdokument rinosinuit – Läkemedelsverket – www.lakemedelsverket.se/behandling-och-forskrivning
https://webcache.googleusercontent.com/search?q=cache:ehneYjXKdjgJ:https://www.lakemedelsverket.se/49f6b1/globalassets/dokument/behandling-och-forskrivning/behandlingsrekommendationer/bakgrundsdokument/bakgrundsdokument-rinosinuit.pdf+&cd=4&hl=sv&ct=clnk&gl=se&client=firefox-b-d
Epidemiologi och definition av akut och kronisk sinuit hos barn och vuxna. I en metaanalys från 2006 analyserades fyra studier på vuxna, som sammantaget visade att bakterieodlingar som riktas mot mellersta näsgången (området mellan den nedre och mellersta näsmusslan där maxillar-, ethmoidal-, och frontalsinus tömmer sig), gav en representativ bakteriell
profil av de bakterier som fanns i punkterade sinus (14). I genomsnitt var överensstämmelsen 87 % (14). Vad gäller barn finns endast enstaka studier. I en studie från Taiwan jämfördes endoskopiska odlingar från mellersta näsgången med punktion från maxillarsinus i 41 bakterieodlingspar, där man fann en överensstämmelse mellan de båda odlingarna i 78 % av fallen (15). Radiologi rekommenderas endast om det finns kliniska tecken till allvarliga komplikationer till bakteriell rinosinuit eller om ställningstagande till kirurgisk åtgärd behövs. En utebliven förbättring eller försämring av symtom efter 48 timmars behandling med intravenös antibiotika är också ett argument för radiologi.
Se också – https://www.internetmedicin.se/behandlingsoversikter/infektion/rinosinuit/ och https://vardgivare.skane.se/vardriktlinjer/oron-nasa-hals/ako/sinuit/
Mast cell activation syndrome, Inflammaging and Tinnitus
MCAS: Effects on eyes, ears, nose and mouth https://www.mastattack.org/2014/10/mcas-effects-on-eyes-ears-nose-and-mouth/
Mast Cell Activation Syndrome and Histamine: When Your Immune System Runs Rampant https://hoffmancentre.com/mast-cell-activation-syndrome-histamine-immune-system-runs-rampant/
“..Conditions Associated with Mast Cell Activation Syndrome
Because MCAS is a chronic, multisystem, multisymptom condition with an inflammatory theme, it’s been associated with a number of conditions and diseases, including:
Chronic inflammatory response syndrome
Irritable bowel syndrome
Gut dysbiosis – the gut is rich in mast cells and home to over 70% of the immune system. Parasites, bacteria, fungi, and parasites can all trigger gut mast cells.
Obesity
Diabetes
Asthma and allergies
Autism
Autoimmune diseases (such as lupus, rheumatoid arthritis, and Hashimoto’s)
Candida overgrowth
Celiac disease
Parasite infections
Skin conditions such as eczema and psoriasis
Food intolerances and allergies
Gastroesophageal reflux (GERD)
Infertility and endometriosis
Chemical and medication sensitivities
Postural orthostatic hypotension (POTS)
CIRS – exposure to mold mycotoxins is a potent stimulator of mast cell activation
Migraines
Depression
Fibromyalgia
Fungal infections
Tinnitus
Multiple Sclerosis
Cancer
In general, inflammation accompanies MCAS and most of its coinciding or associated illnesses. If you are struggling to get one of these illnesses under control, there’s a possibility MCAS could be causing further complications.
It’s a good idea to check for MCAS if you have any of the above conditions and vice versa.
You can take our Hoffman Centre for Integrative Medicine MCAS Questionnaire HERE.
Neurovascular Inflammaging in Health and Disease https://www.mdpi.com/2073-4409/9/7/1614
(goggle on “mast cell Inflammaging” = pictures also!
”Aging is characterized by a chronic low-grade sterile inflammation dubbed as inflammaging, which in part originates from accumulating cellular debris. These, acting as danger signals with many intrinsic factors such as cytokines, are sensed by a network of pattern recognition receptors and other cognate receptors, leading to the activation of inflammasomes. Due to the inflammasome activity-dependent increase in the levels of pro-inflammatory interleukins (IL-1β, IL-18), inflammation is initiated, resulting in tissue injury in various organs, the brain and the spinal cord included. Similarly, in age-related diseases of the central nervous system (CNS), inflammasome activation is a prominent moment, in which cells of the neurovascular unit occupy a significant position. In this review, we discuss the inflammatory changes in normal aging and summarize the current knowledge on the role of inflammasomes and contributing mechanisms in common CNS diseases, namely Alzheimer’s disease, Parkinson’s disease, amyotrophic lateral sclerosis and stroke, all of which occur more frequently with aging …” See print out
From Dr Jill = Mast Cell Activation Syndrome: Here’s What You Need to Know When Histamine Goes Haywire https://www.jillcarnahan.com/2016/10/31/mast-cell-activation-syndrome-mcas-when-histamine-goes-haywire/
NB excellent pratical description
Mast cells and histamine are triggering the NF-κB-mediated reactions of adult and aged perilymphatic mesenteric tissues to acute inflammation https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5191886/
Inflammaging in Skin and Other Tissues – The Roles of Complement System and Macrophage
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4082166/
Immunosenescence, Inflammaging, and Their Implications for Cancer and Anemia https://www.researchgate.net/publication/334782298_Immunosenescence_Inflammaging_and_Their_Implications_for_Cancer_and_Anemia
MCAS: Effects on eyes, ears, nose and mouth https://www.mastattack.org/2014/10/mcas-effects-on-eyes-ears-nose-and-mouth/ – EDUCATING PEOPLE ABOUT LIFE WITH MAST CELL DISORDERS
… Hearing abnormalities are often found in MCAS patients. They include hearing loss, ringing of the ears, and sensitivity to sound. This is thought to be from sclerosis of the innter ear bones or tympanic membrane, which has been known to occur coincidentally with mast cell disease since the 1960’s. Deterioration of the canal hairs and auditory nerve is also suspected in some patients. Tinnitus is likely from mediator release causing overstimulation of the hair cells and auditory nerve fibers. The most common finding by audiologists is sensorineural hearing loss of unclear origin.
Kronisk Rinosinuitis tKRS) och inflammaging
Do Aging Factors Influence the Clinical Presentation and Management of Chronic Rhinosinusitis?
https://journals.sagepub.com/doi/abs/10.1177/0194599817691258?journalCode=otoj
“Age-dependent decrease in the levels of the S100 family proteins (https://pubmed.ncbi.nlm.nih.gov/32564786/ – https://www.researchgate.net/requests/r81831782) involved in epithelial proliferation, repair, and defenses combined with chronic inflammation might lead to an increased risk of abnormal microbial colonization and loss of microbiota diversity. Ultimately, these changes could have the potential to alter the physiopathology of CRS in the elderly.”
S100 family proteins in inflammation and beyond https://www.researchgate.net/publication/340723108_S100_family_proteins_in_inflammation_and_beyond printout requeted
NO and ….
Nitric oxide and the paranasal sinuses – Lundberg – https://pubmed.ncbi.nlm.nih.gov/18951492/
2020 -> https://www.researchgate.net/publication/23414765_Nitric_Oxide_and_the_Paranasal_Sinuses
Upptäckten inom paranasala bihålor för produktion av kväveoxid (NO) har förändrat de traditionella förklaringarna av sinusfysiologi. Denna översyn artikeln rapporterar den pågående undersökningen av sinus fysiologi som börjar med upptäckten av NO gasproduktion i paranasal bihålorna som inträffade 1995, och den inverkan som konstaterandet har haft både i de grundläggande vetenskap och kliniska arenor. Det visades att friska paranasal sinus epitel uttrycker en inducerbara NO syntas som kontinuerligt genererar stora mängder NO, en pluripotent gasformiga budbärare med potent vasodilaating, och antimikrobiell verksamhet. Detta NO kan mätas noninvasively i nasalt utandad andedräkt. ROLLEN AV NO i bihålorna är sannolikt att förstärka lokala värd försvar mekanismer via direkt hämning av patogentillväxt och stimulering av mucociliary verksamhet. NO-koncentrationen i en frisk sinus överstiger de som behövs för antibakteriella effekter in vitro. Hos patienter med primär ciliär dyskinesi (PCD) och i cystisk fibros är nasala NO extremt låg. Denna defekt NO generation sannolikt bidrar till den stora mottaglighet för kronisk bihåleinflammation hos dessa patienter. Dessutom är det låg-nasala NO av diagnostiskt värde särskilt i PCD, där nasal NO är mycket låg eller frånvarande. Spännande, NO gas från näsan och bihålorna inhaleras med varje andetag och når lungorna i en mer utspädd form för att förbättra pulmonell syreupptagning via lokala vasodilatation. I denna mening NO kan betraktas som en ”aerocrine” hormon som produceras i näsan och bihålorna och transporteras till en distala platsen för åtgärder med varje inandning.
The new organic nitrate 2-nitrate-1,3-diocthanoxypropan (NDOP) induces nitric oxide production and vasorelaxation via activation of inward-rectifier potassium channels (KIR).
https://europepmc.org/article/med/33038483
“… CONCLUSION:Bioactivation of NDOP involves functional XOR, and this new organic nitrate elicits vasorelaxation via NO-cGMP-PKG signaling and activation of KIR channels. Future studies should further characterize the underlying mechanism and evaluate the therapeutic benefits of chronic NDOP treatment in relevant cardiovascular disease models.”
Aso https://www.researchgate.net/scientific-contributions/Jon-O-Lundberg-55346542
Vargata
“En akut bakteriell bihåleinflammation (sinuit) kan yttra sig genom att var (pus) läcker ut från käkbihålan till näshålan. En sådan rännil av var brukar benämnas ”vargata” och kan ses vid inspektion av näshålan efter avsvällning av slemhinnan. Varet innehåller ofta en kombination av bakterier och vita blodkroppar” https://www.vardhandboken.se/undersokning-och-provtagning/nasofarynxodling/infektioner-och-odling/
Högt diagnostiskt värde: Ensidig värk över käkhålan. med tryck eller värk mot. överkäkständer. Ensidig purulent snuva. Vargata i näsan. Illaluktande sekret.
https://slideplayer.se/slide/2311090/
“Vargata i epifarynx”
Länkar
https://lakemedelsboken.se/kapitel/andningsvagar/oron-_nas-_och_halssjukdomar.html Rinosinuit
https://www.netdoktorpro.se/oron-nasa-hals/medicinska-oversikter/akut-rinosinuit/
https://www.praktiskmedicin.se/sjukdomar/bihaleinflammation-sinuit-bakteriell-rinosi/
Internationella behandlingsriktlinjer för rinosinuit ger bra vägledning –
https://lakartidningen.se/wp-content/uploads/OldWebArticlePdf/1/10648/LKT0845s3202_3206.pdf
https://lakartidningen.se/klinik-och-vetenskap-1/2008/10/internationella-behandlingsriktlinjer-for-rinosinuit-ger-bra-vagledning/
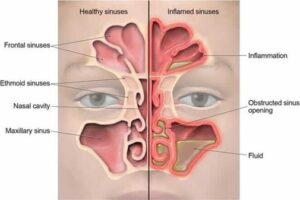
Sinuit, speciellt maxillaris typ 2 utan symptom
Svensk hemsida: Rinosinuit https://www.internetmedicin.se/behandlingsoversikter/infektion/rinosinuit/?fbclid=IwAR1aFke_ZlfeEv_acZ9wEWFyfrPn0EoRhVWZJacZcIYnlT-pfXsgJdny4IY
https://medicarehealth.co.za/care/allergies/sinusitis/
https://teachmeanatomy.info/head/organs/the-nose/paranasal-sinuses/
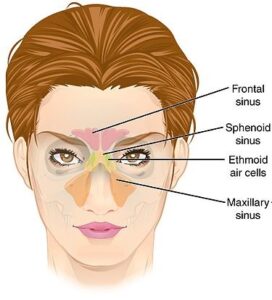
“The maxillary sinus is the largest of the paranasal sinuses. The two maxillary sinuses are located below the cheeks, above the teeth and on the sides of the nose. The maxillary sinuses are shaped like a pyramid and each contain three cavities, which point sideways, inwards, and downwards” https://www.healthline.com/human-body-maps/maxillary-sinus#1
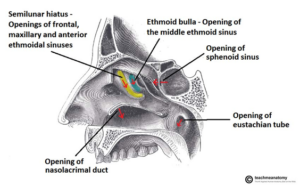
“The paranasal sinuses drain into the nasal cavity. The frontal, maxillary and anterior ethmoidal sinuses open into the middle meatus. The location of this opening is marked by the semilunar hiatus, a crescent-shaped groove on the lateral walls of the nasal cavity.” https://teachmeanatomy.info/head/organs/the-nose/nasal-cavity/
“The maxillary sinus drains into the middle meatus by means of the semilunar hiatus. The floor of the maxillary sinus is slightly below the level of the nasal cavity, and it is related to the upper teeth (varying from teeth 3 to 8 to teeth 6 to 8). Maxillary sinusitis is frequently accompanied by toothache.” https://www.dartmouth.edu/~humananatomy/part_8/chapter_52.html
“It is not uncommon for people with sinus pressure to experience middle ear blockage due to congestion of the eustachian tubes. This swelling is most commonly caused by a sinus infection, a cold, or allergies. These conditions can cause the inner ear membranes to swell and block the tubes” https://www.everydayhealth.com/ear-nose-throat/eustachian-tube.aspx
Maxillary Sinusitis
Maxillary sinus can be found below the eyes, on the cheekbone. More often than not, infection can be developed in this area.The most common symptoms is migraine, pain on the upper part of the teeth and pounding pressure below the eyes.Other symptom includes redness of the eyes and some parts of the cheekbone, chills, fever and change in vision. The infection can also affect your chewing because this type of sinusitis has connections to the teeth. It would be hard to chew because the pain can affect the upper part of the teeth.
Different Types of Maxillary Sinusitis. There are two types of maxillary infection. The first type is acute sinusitis. This can be treated easily because clinical symptoms such as pain in the cheek or maxillary teeth are obvious and can easily be resolved with antibacterial medicines.
On the other hand, chronic sinusitis is harder to treat because the clinical symptoms are sometimes not present. During this time, polyps are forming in the sinus. Chronic maxillary surgery can be the best treatment in this case because of the presence of polyps. Polyps are grape-lie swollen lining of the sinus that blocks the air passage. The patient can only get rid of it through surgery. During the surgery, the patient should be totally unconscious because of the sensitivity of the process.” https://ehr.wrshealth.com/live/patient_v2/instructions.php?id=2427145&iid=6040
Recurrent sinusitis and impairment of eustachian tube function in air passengers and crew
https://pubmed.ncbi.nlm.nih.gov/2386456/
“Chronic and recurrent sinusitis, and thus impaired tubular function, are usually caused by isolated lesions of the ethmoid cells. Purulent nasal secretions are transported over the openings of the tubes into the epipharynx. Inflammation and swelling of the mucosa of the tube openings causes stenosis or blockage. Inflammatory foci, usually hidden in the anterior ethmoid cell system, are not always apparent in a plain film of the paranasal sinuses. They appear only in a computed-tomography scan or in a conventional tomogram. Once the diagnosis has been made, a simple, guided endoscopic procedure suffices to alleviate a stenosis, open inflamed ethmoid cells, and restitute ventilation of the nasal sinuses and, thus, tubal function. Radical procedures on the maxillary and frontal sinuses, and plastic operations on deviated nasal septa (which impair the function of the nose and the nasal sinuses only in extreme cases), are thus often unnecessary. Septum deviations are irrelevant to the fitness-to-fly of air personnel as long as the tube and the ventilation of the sinuses function freely. The Valsalva maneuver with otoscopic visualization of the excursion of the eardrum is the most reliable test of tubal function. Tympanometry is used mainly for documentation”.
Mer om Sinus problem
The silent sinus syndrome – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3731971/ “The silent sinus syndrome (SSS) involves painless facial asymmetry and enophthalmos, which is the result of chronic maxillary sinus atelectasis. In most cases, it is diagnosed clinically, however, using the characteristic imaging features including maxillary sinus outlet obstruction, sinus opacification, and sinus volume loss caused by inward retraction of the sinus walls. Obstruction of the maxillary ostium appears to play a critical role in the development of SSS. Treatment involves functional endoscopic surgery.
“Acid reflux can sometimes actually contribute to sinusitis! That is to say, the acid can travel all the way up to your nose and sinuses (for instance, while you are lying down asleep), and this acid can inflame the nose and sinus linings. This problem is more common in children — but it may also be seen in adults.” https://www.beckerentandallergy.com/sinus/gerd
Tyst Sinus Syndrome
Diagnosis and Management of Silent Sinus Syndrome – https://www.aao.org/eyenet/article/diagnosis-management-of-silent-sinus-syndrome
And https://www.health.harvard.edu/a_to_z/chronic-sinusitis-in-adults-a-to-z
https://pubmed.ncbi.nlm.nih.gov/30468775/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4855421/
2020-11-08
Sinuitis & Örontrumpeten
Is Chronic Rhinosinusitis and Status of Pharyngeal End of Eustachian Tube Link-Up: All Smoke No Fire? https://webcache.googleusercontent.com/search?q=cache:9Bw_Foc51PoJ:https://www.ijcmr.com/uploads/7/7/4/6/77464738/_fijcmr_639_may_26.pdf+&cd=13&hl=sv&ct=clnk&gl=se&client=firefox-b-d
ABSTRACT Introduction: Chronic Rhinosinusitis is one of the commonly encountered problems in otorhinolaryngology practice. Aim was to study the effect of Chronic Rhinosinusitis on pharyngeal end of Eustachian tube opening by nasal endoscopy, and to emphasize the need for proper diagnostic endoscopic evaluation in Eustachian tube dysfunction. Material and Methods: Eighty three patients of Chronic Rhinosinusitis, in the age group of 18-65 years, were identified. Eighty three patients were selected as control group having asymptomatic deviated nasal septum and no subjective or objective evidence of chronic rhinosinusitis. The changes at the pharyngeal end of the Eustachian tube were assessed by endoscopy, according to the types of changes, graded from I to V. Results: Evaluation revealed that Chronic Rhinosinusitis causes changes at the pharyngeal end of the Eustachian tube in 81.92% (68/83) cases. Type I (normal Eustachian tube) was seen in 18.08% (15/83). Type II changes were seen in 71% (59/68) cases, type III changes were seen in 13.23% (9/68) cases. In control group normal ET orifice was seen in 74.69%, Type II changes were seen in 18.07% and type III changes in 7.22% cases. Conclusion: Chronic Rhinosinusitis cause changes at the pharyngeal end of Eustachian tube, in the form of congestion, mucosal oedema and blockage of tube. This in turn can lead to middle ear disease. Nasal endoscopy should be done in all the cases of chronic rhinosinusitis, to examine nose, nasopharynx and pharyngeal end of Eustachian tube.
.. When Your Eustachian Tubes Malfunction – https://www.everydayhealth.com/ear-nose-throat/eustachian-tube.aspx
A number of things can go wrong with your eustachian tubes and middle ear, including:
Blockage due to swelling. It is not uncommon for people with sinus pressure to experience middle ear blockage due to congestion of the eustachian tubes. This swelling is most commonly caused by a sinus infection, a cold, or allergies. These conditions can cause the inner ear membranes to swell and block the tubes. A blocked eustachian tube cannot circulate air or drain mucus as it should
Mechanical blockage. Sometimes overgrowth of tissues in the back of the nose (such as nasal polyps or the adenoids) can cause ear blockage by obstructing the eustachian tube opening. On rare occasions, a tumor can cause a blockage.
Otitis media (middle ear inflammation or infection). When sinus congestion leads to a blocked eustachian tube, fluid can accumulate in the middle ear and cause it to become inflamed. Similarly, if you have a bacterial sinus infection that spreads into your eustachian tubes, it can cause a middle ear infection, which leads to swelling and more fluid buildup. Otitis media is associated with ear pain and pressure.
Ruptured eardrum. If too much fluid builds up in your inner ear, it could tear your eardrum.
Middle Ear and Sinus Problems https://www.skybrary.aero/index.php/Middle_Ear_and_Sinus_Problems
“Causes of Blockage to the Middle Ear & Sinuses:
Apart from physiological reasons, the anatomic causes of blocked Eustachian tubes and ostia are practically identical and often the two events will occur together.
Most commonly, these causes are both bacterial and viral infections such as colds and flu; however, blockages can also occur as a reaction to allergies and various diseases. Because, in both the middle ear and the sinuses, a blockage means that mucous cannot be removed, it is possible for bacteria to grow in this mucous, causing further infection, such as sinusitis, and therefore prolonging the problem.
WHY & HOW YOUR SINUSITIS & TINNITUS MAY BE CONNECTED – https://www.sinusofsf.com/sinusitis/sinusitis-tinnitus-connected/
“Sinusitis and tinnitus are a troublesome twosome; however, their connection isn’t particularly obvious. Sinusitis can cause, worsen, or exasperate tinnitus, a ringing in the ears typically associated with hearing loss and exposure to overly loud noises. But if sinusitis-related tinnitus doesn’t originate with hearing damage, what does cause it? Can tinnitus be temporary? How do you treat sinusitis & tinnitus? Sinus Solutions of South Florida is here to answer these questions and more.
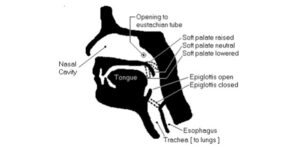
HOW CAN A SINUS INFECTION AFFECT YOUR EARS? Most sinusitis-related ear problems, including tinnitus, are caused by the congestion that occurs during a sinus infection. To better understand this phenomenon, let’s take a second to review a few facts about sinusitis. Sinusitis most frequently occurs when a virus or bacteria irritates the tissues of your sinus cavities. This irritation can lead to swelling which, in turn, can lead to mucus buildup and congestion.
Your sinus cavities and ears are interconnected systems, so congestion in the sinuses can create ear congestion, as well. Congestion in the ear may block the tube — known as the Eustachian Tube — that connects the middle ear to the outer ear and helps regulate pressure within the ear. When the Eustachian Tube is blocked, the pressure is allowed to build up around the eardrum, which is ultimately what causes ringing in the ears, aka tinnitus. Whether you have an acute sinus infection or a sinus infection that won’t go away, so long as the congestion is severe enough, it can cause tinnitus.
PULSATILE TINNITUS AND SINUS CONGESTION While not common, pulsatile tinnitus — tinnitus during which patients claim to hear a sound similar to and in rhythm with their heartbeat — may occur. This type of tinnitus is typically caused by an increase in blood flow.
SINUSITIS & TINNITUS: FINDING SINUS EAR RINGING TREATMENT Fortunately, sinusitis-related tinnitus tends to go away with treatment of the sinus infection. As a minimally-invasive procedure, balloon sinuplasty can be performed in-office in less than 20 minutes on patients with a medical sinus obstruction. During this procedure, your otolaryngologist uses an endoscope to place a tiny balloon within your sinus cavity. Once infla ted, this balloon can expand your sinuses, restoring drainage to areas that were previously blocked or too small for mucus to flow properly.
The procedure has the added benefit of requiring little-to-no recovery time, and the majority of balloon sinuplasty before and after testimonies speak to patients finding years of much-needed sinus relief”.
Mer om örontrumpeten och dess funktioner
Se http://carism.se/projekt-carism/a-multidisciplinary-overview-of-the-tinnitus-syndrome-fields/overview-of-some-of-the-tinnitus-syndrome-approaches/
Mellanörats komplexa, problematiska ”jobb”
Se http://carism.se/projekt-carism/a-multidisciplinary-overview-of-the-tinnitus-syndrome-fields/overview-of-some-of-the-tinnitus-syndrome-approaches/
Ear fullness
Why Does My Ear Feel Clogged? – https://www.healthline.com/health/why-does-my-ear-feel-clogged – https://www.healthline.com/health/why-does-my-ear-feel-clogged#_noHeaderPrefixedContent
“1. An Eustachian tube blockage is one possible cause of a clogged ear. The Eustachian tube connects the middle ear to the throat. Fluid and mucus flows from the ear to the back of the throat through this tube, where it’s swallowed. But instead of flowing down the throat, fluid and mucus can sometimes become trapped in the middle ear and clog the ear. This blockage usually accompanies an infection, such as the common cold, influenza, or sinusitis. Allergic rhinitis can also cause a blockage in the Eustachian tube.”
“4. Acoustic neuroma is a benign growth that develops on the cranial nerve leading from the inner ear to the brain. These tumors are usually slow-growing and small. However, as they become larger, they can put pressure on nerves in the inner ear. This can cause a clogged ear, hearing loss, and a ringing in the ear.”
Treatments for a clogged ear
Although a clogged ear is an annoying distraction, it’s usually treatable with home remedies.
- Use the Valsalva maneuver – This simple trick helps open your Eustachian tube. To perform this maneuver, take a deep breath and pinch your nose. With your mouth closed, attempt to exhale gently through your nose. This should create enough pressure to “pop” or unclog the ear. Don’t blow too hard to avoid damaging your eardrum. Once your Eustachian tube opens, chew gum or suck on hard candy to keep it opened.
- Inhale steam – Turn on a hot shower and sit in the bathroom for 10 to 15 minutes. The steam from the hot water helps loosen mucus in the ear. Another option is placing a hot or warm washcloth over your ear.
- Dislodge trapped fluid – Insert your index finger into the affected ear and gently move your finger up and down. This technique helps remove trapped fluid. A hair dryer on a low heat setting held a few inches from your ear might also help dry fluid in the ear.
- Take over-the-counter medication – Over-the-counter (OTC) medication can treat a clogged ear caused by sinus drainage, colds, or allergies. Take cold or sinus medication containing a decongestant, or take an antihistamine. Make sure to follow the directions on the label.
- Ear drops – An earwax removal kit (Debrox Earwax Removal Kit or Murine Ear Wax Removal System) can soften and flush earwax from the ears. You can also place two or three drops of warm mineral oil, baby oil, or hydrogen peroxide into your ear using a medicine dropper. Keep your head tilted for a few seconds after applying the drops to flush wax from the ear.
https://www.healthgrades.com/right-care/ear-nose-and-throat/ear-fullness
“Ear fullness is usually the result of a cold or flu that blocks the Eustachian tube and may lead to ear infection. In some cases, ear fullness may be a symptom of severe infection of the bone behind the ear, which is a serious or life-threatening condition that should be evaluated immediately in an emergency setting”.
NB Below is a cut-through view of a human head:
https://gofreediving.co.uk/wp-content/uploads/2018/05/Frenzel-techinique-Eric-Fattah.pdf
- The passage that leads to the lungs is called the Trachea. It can be opened or closed by the epiglottis. • The passage that leads to the stomach is called the Esophagus. It can be opened or closed, but it is always closed except during the act of swallowing. • Air flowing in or out of the lungs can be directed by the soft palate. If the soft palate is in the neutral position (as shown above), then air is free to flow through both the nose and the mouth. • If the soft palate is raised, the nasal cavity is sealed off, and air can flow only through the mouth. • If the soft palate is lowered, the mouth is closed off, and air can flow only through the nose. • The openings to the eustachian tubes are in the nasal cavity. The key to equalizing the ears is to force air into the eustachian tubes.
More complex knowledge about Inflammaging
Can be find at http://biopsychosocialmedicine.com/projects/senior-health/senoinflammation-or-inflammaging-or/
* Men ibland utmanar ny kunskap det vi kanske tagit för givet, som visar sig kanske vara destruktivt. Gäller då att kritiskt granska även när det gäller helt nytt perspektiv, se t.ex. Paradigm | Biopsychosocial Medicine eller problemen kring Confirmation bias (i princip = det man redan tror – inom sitt privata/vetenskapliga/kliniska paradigm, tror man är rätt), A huge problem for health care? Confirmation bias, placebo/nocebo vs reductionistic medicine | Biopsychosocial Medicine – Ett stort problem i princip i all utbildning är att många uppfattar de kunskaper (och relaterad praktik) som lärs ut är exakt kunskap, vilket det inte är utan olika grad av ”säker kunskap”. Än värre är om utläraren tror att denna(e) lär ut absolut kunskap utan olika grad av bristfällig som vederbörande utlärare själv mer eller mindre förstått. OBS det är inte svart eller vitt, går man över en gata med trafik hela tiden så skall man inte gå rakt ut utan att se sig för! Samma gälle r all typ av inlärning – det gäller att se sig för och kritiskt granska innan man accepterar ”paradigmet” som lärs ut – se ovan länk!
Ytterligare problem är ”när en kliniker säger ”vi använder bara det som är evidensbaserat” utan att uppenbarligen inte känna till hur evidensbegreppet kan definieras men också att det inte sällan gör kliniska insatser ”tandlösa” – eftersom det mesta är inte ens normativt (alltså inte individuellt-kliniskt) empiriskt noggrant undersökt. Uppmanar tvivlande att kolla Evidenced based falsification of data or validation of the individual patient in front of us? | Biopsychosocial Medicine
Länkar
Inflamm-Aging, Cytokines and Aging: State of the Art, New Hypotheses on the Role of Mitochondria and New Perspectives from Systems Biology https://www.researchgate.net/publication/6870555_Inflamm-Aging_Cytokines_and_Aging_State_of_the_Art_New_Hypotheses_on_the_Role_of_Mitochondria_and_New_Perspectives_from_Systems_Biology
https://link.springer.com/article/10.1007/s00005-015-0377-3 – https://pubmed.ncbi.nlm.nih.gov/26658771/
https://cmb.i-learn.unito.it/pluginfile.php/5044/mod_resource/content/1/Minciullo_et_al.pdf
Tool like receptor signaling in “inflammaging”: microRNA as new players https://immunityageing.biomedcentral.com/articles/10.1186/1742-4933-10-11
https://www.research-collection.ethz.ch/bitstream/handle/20.500.11850/221099/2/manuscript.pdf
Cytokines for evaluation of chronic inflammatory status in ageing research: reliability and phenotypic characterisation https://immunityageing.biomedcentral.com/articles/10.1186/s12979-019-0151-1
Altered microRNA expression links IL6 and TNF-induced inflammaging with myeloid malignancy in humans and mice
Inflammaging is defined as low-grade chronic systemic inflammation established during physiological aging. Altered levels of proinflammatory cytokines (e.g., IL-6 and TNF-α), acute-phase reactants (C-reactive protein [CRP]), and decreases in IL-10 impair the maintenance of immunological homeostasis. Can Exercise Be an Immunotherapy? https://www.medscape.com/viewarticle/809935_7
Macrophages in age-related chronic inflammatory diseases – https://www.nature.com/articles/npjamd201618
Chronic Inflammation (Inflammaging) and Its Potential Contribution to Age-Associated Diseases
https://academic.oup.com/biomedgerontology/article/69/Suppl_1/S4/587037
Source of Chronic Inflammation in Aging https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5850851/
… During physiological aging process, a low-grade chronic systemic inflammation, called inflammaging, develops and impairs the maintenance of immunological homeostasis, in which there are high levels of Creactive protein (CRP), proinflammatory cytokines as IL-6, in addition to low level of anti-inflammatory cytokines
https://www.researchgate.net/publication/326612330_Inflammaging_a_new_immune-metabolic_viewpoint_for_age-related_diseases